This article was written by Dr Michelle Ní Raghallaigh, Sleep Specialist and Neuroscientist PhD.
Most of us have experienced the impact of stress on our sleep – that late-night upsetting phone call, a work email just before bed, or a triggering argument with a loved one. The next thing we know, our minds are ‘racing’ so much that we can’t fall asleep, or we wake up in the middle of the night in a state of ‘high alert’.
But how exactly does this happen?
Here we’re going to show you how exactly this happens because by empowering you with this knowledge, the better equipped you’ll be to not only know what’s going on, but also how to reduce the impact of stress on our sleep.
First, let’s define ‘stress’ (for this article I’m talking about stress in the short-term). In the scientific literature, the term ‘stress’ refers to experiences considered to be emotionally or physiologically demanding, and to our adaptive response to that experience. This adaptive response involves the autonomic nervous system, particularly the sympathetic nervous system, stimulating the release of adrenaline (epinephrine) and noradrenaline (norepinephrine). These increase our heart rate and body temperature, both of which make it harder to fall asleep and transition from lighter to deeper sleep stages.
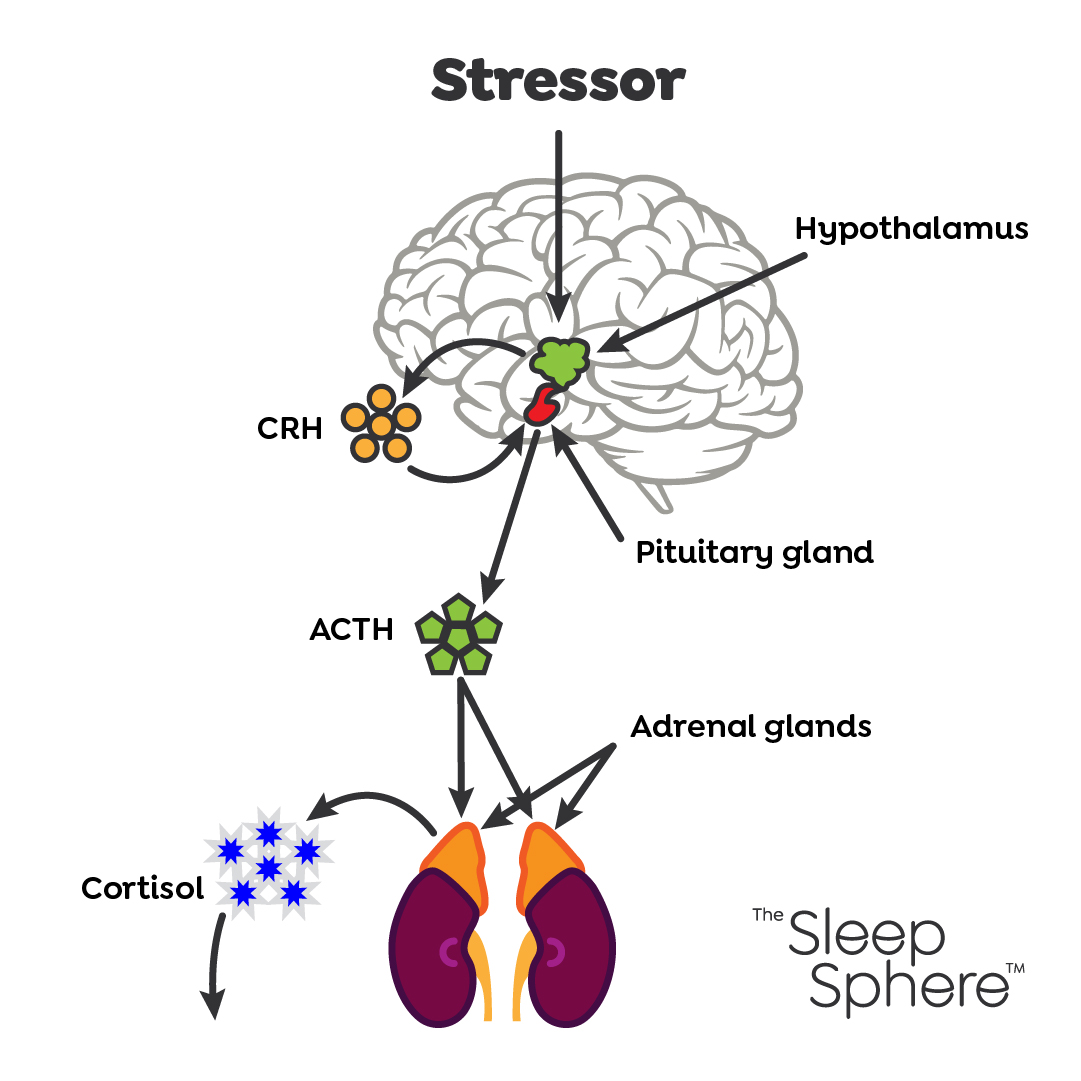
The stress response also involves the hypothalamic-pituitary-adrenal (HPA) axis, a hormonal system that mediates the impact of stress by regulating multiple physiological processes (Lo Martire et al., 2020). More specifically, stress causes the brain’s hypothalamus to release corticotropin-releasing hormone (CRH), which triggers the pituitary gland to release adrenocorticotropin hormone (ACTH). This hormone in turn triggers the release of cortisol from the adrenal glands (located just above our kidneys) into the bloodstream (Clow et al., 2004).
Cortisol is associated with increased hyperarousal i.e. elevated cognitive, emotional, and physiological activity. Increased HPA activity and cortisol are specifically known to fragment our sleep, with a reduction in our deep slow-wave sleep and increased wakefulness. Indeed, the preceding evening’s cortisol levels correlate with awakenings that night (Rodenbeck et al., 2002).
How does cortisol behave in people with insomnia compared to those who don’t? Typically, cortisol is normally at its highest in the morning; this morning cortisol rise is what helps get us out of bed in the morning! Cortisol levels then gradually drop as the day goes by. However, in those with insomnia, higher levels of cortisol are shown in the morning time and throughout the day including the evening time, compared to those without insomnia (Grimaldi et al., 2021).
Stress can precipitate a vicious perpetuating cycle: stress causes heightened HPA axis activity, which negatively affects our sleep. Then this fragmented disrupted sleep in itself negatively affects the HPA axis (poor sleep becomes stressful in its own right), leading to a maintenance and progression of the sleep disruption into the longer-term (Lo Martire et al., 2020) i.e. transition into chronic insomnia.
Now that we know there is this vicious cycle going on, what can we do about it?
The good news is that there is a way of dealing with the spiralling nature of stress and sleep disruption: we nip things in the bud! We can catch things before they deteriorate, using CBTI.
CBTI is recommended as the first-line treatment for insomnia worldwide, and studies have shown that it helps prevent the transition from acute to chronic insomnia (Yang et al., 2023).
CBTI is designed to break the vicious cycle of insomnia that perpetuates poor sleep into something more entrenched. In addition to the physiological and circadian components of CBTI, techniques such as worry techniques, guided imagery, and progressive muscle relaxation all help bring down our levels of hyperarousal.
What if you find yourself beginning to struggle with your sleep? Even if you’re experiencing sleep loss for a short period of time e.g. a few nights or weeks, it may be worth considering CBTI support for this. Studies show that CBT-I may help prevent insomnia and suggest that it is an effective tool to promote mental and physical health during stress (Cheng et al., 2020).
Many people suffering from sleep loss temporarily feel that they have to just ‘put up with it’ until things improve. Rather than suffering alone and unnecessarily, and feeling like you shouldn’t look for support unless it’s been going on for a long time, there is an option for evidence-based tailored support available to help you.
By stopping insomnia in its tracks, we’ll be buffering ourselves from any stress that could come our way in the future.
Here are some of my quick tips for reducing hyperarousal during times of stress:
- Get things out of your head and onto paper. Writing down your thoughts and worries for even a few minutes each evening signals to your brain that you’ve taken action on those worrying thoughts.
- Try Progressive Muscle Relaxation (PMR), a system of alternating contracting and relaxing different muscles. Stress increases muscle tension, which triggers sleeplessness. This technique reduces muscle tension, making sleep easier. Please email us if you would like access to our audio guide for this.
- Guided Imagery is clinically recommended for insomnia, some options including a woodland walk and a beach stroll are here.
- Consider a therapeutic massage to bring down that muscle tension! The following expert in Shiatsu and Japanese massage is highly recommended: https://www.salus-wellness.com/practictioners/yumi-matsumoto/
For compassionate, science-led support for your sleep and insomnia, get in touch here
